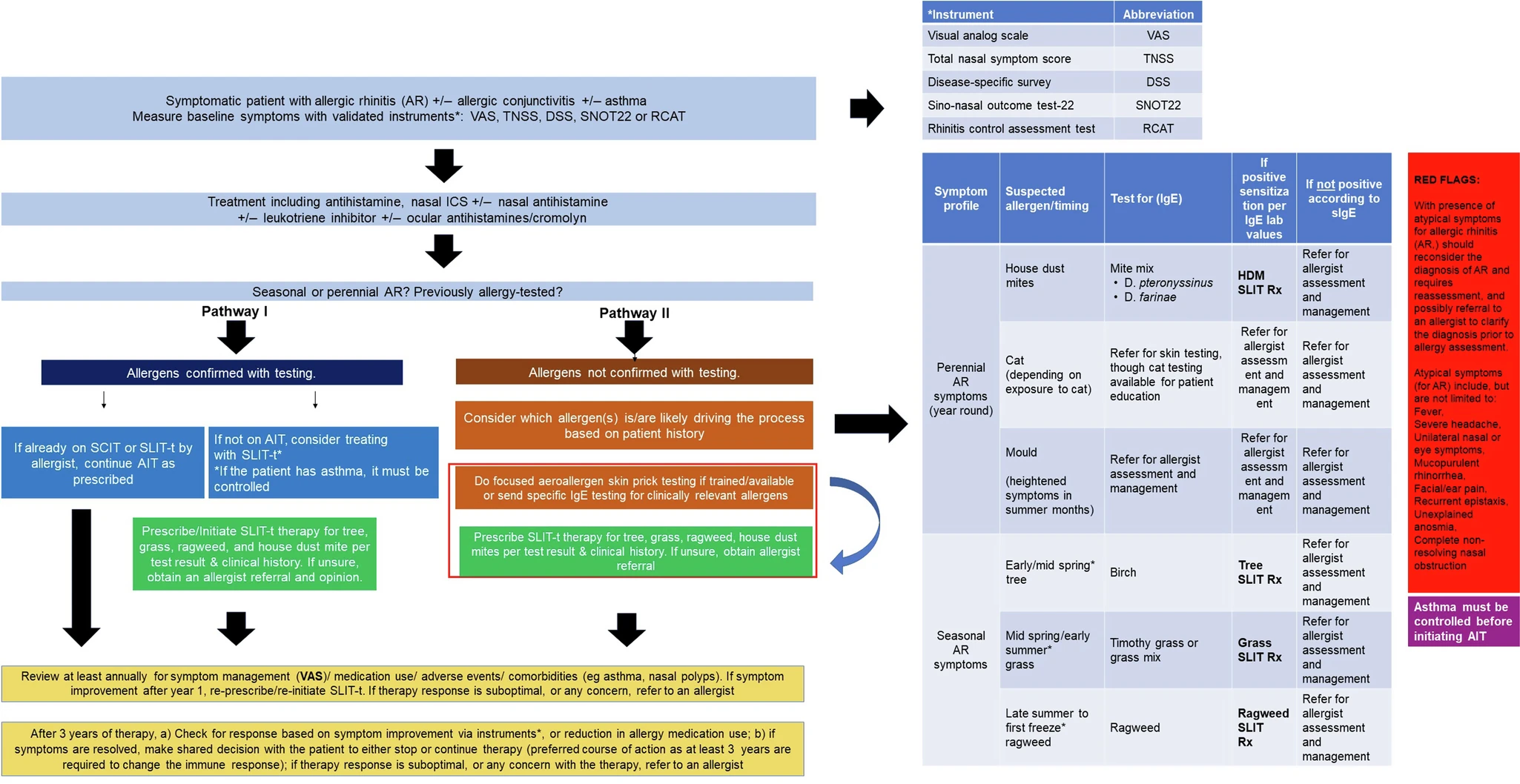
Bustos, G., Sanchez-Gonzalez, M.A., Grogan, T. et al. npj Prim. Care Respir. Med. 34, 22 (2024). https://doi.org/10.1038/s41533-024-00380-zAbstract
Allergic rhinitis (AR), a condition characterized by sensitivity to allergens leading to poor quality of life, including disrupted sleep, reduced vitality, lowered mood, changes in blood pressure limited frustration tolerance, impaired focus, decreased performance in academic and professional settings, and millions of missed work and school days every year. Approximately 20–40% of individuals in the United States are affected by AR, which carries notable clinical and financial burdens. Interestingly, there is a strong link between AR and asthma to the extent that countries with a high prevalence of rhinitis have asthma rates ranging from 10% to 25%. Research has indicated that Allergen Immunotherapy (AIT) is associated with improved AR symptoms, a potential to resolve the AR over time, a decreased likelihood of asthma exacerbations and incidence of pneumonia in individuals with concurrent asthma, which are advantages that persist for years even after the cessation of treatment.
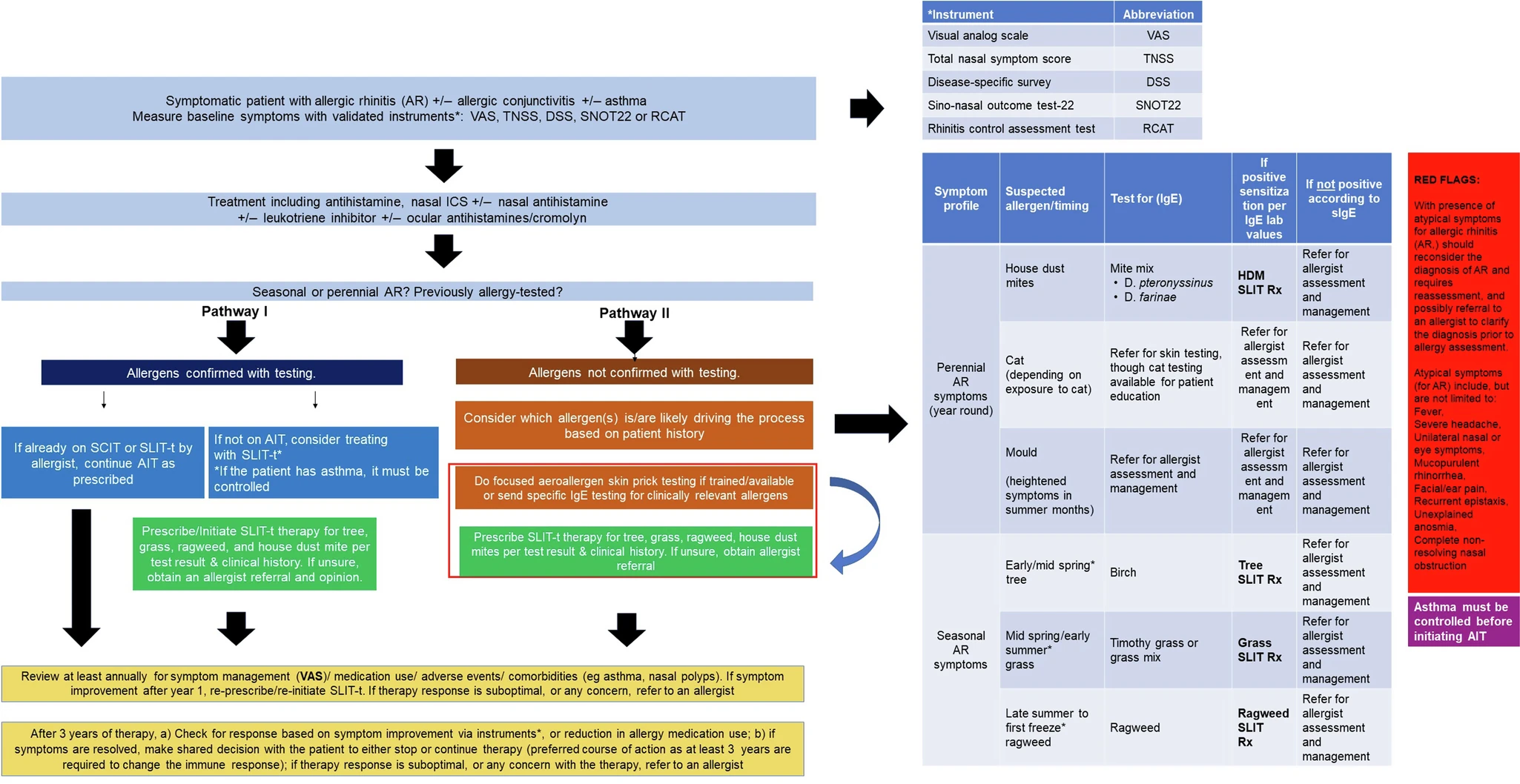 |
| Proposed algorithm for prescribing allergen immunotherapy in the primary care setting. |
Although patients presenting with allergies are first seen and treated in the primary care setting, gaps in training and the lack of available guidance for primary care practitioners have significantly impacted the quality of care for these patients with persistent AR symptoms, resulting in inefficient use of healthcare resources.