Background
Asthma is a heterogeneous disease; therefore, biomarkers that can assist in the identification of subtypes and direct therapy are highly desirable. Asthma is a chronic inflammatory disease that leads to changes in the extracellular matrix (ECM) by matrix metalloproteinases (MMPs) degradation causing fragments of type I collagen that is released into circulation.
Objective
Here, we asked if MMP-generated type I collagen (C1M) was associated with subtypes of asthma.
Methods
C1M was serologically assessed at baseline in the adult participants of the All Age Asthma study (ALLIANCE) (n = 233), and in The Prospective Epidemiological Risk Factor study (PERF) (n = 283). In addition, C1M was assessed in mice sensitized to ovalbumin (OVA) and challenged with OVA aerosol. C1M was evaluated in mice with and without acute neutrophilic inflammation provoked by poly(cytidylic-inosinic) acid and mice treated with CP17, a peptide inhibiting neutrophil accumulation.Results
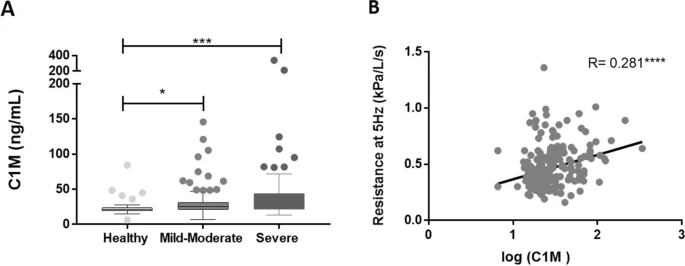
Serum C1M was significantly increased in asthmatics compared to healthy controls (p = 0.0005). We found the increased C1M levels in asthmatics were related to blood neutrophil and body mass index (BMI) in the ALLIANCE cohort, which was validated in the PERF cohort. When patients were stratified into obese (BMI > 30) asthmatics with high neutrophil levels and uncontrolled asthma, this group had a significant increase in C1M compared to normal-weight (BMI < 25) asthmatics with low neutrophil levels and controlled asthma (p = 0.0277). C1M was significantly elevated in OVA mice with acute neutrophilic inflammation compared to controls (P = 0.0002) and decreased in mice treated with an inhibitor of neutrophil infiltration (p = 0.047).
Conclusion & clinical relevance
C1M holds the potential to identify a subtype of asthma that relates to severity, obesity, and high neutrophils. These data suggest that C1M is linked to a subtype of overall inflammation, not only derived from the lung. The link between C1M and neutrophils were further validated in in vivo model.
Trial registration
(ALLIANCE, NCT02419274).