Anton Olsson, Kathryn Steel, Rachael Cooper, Ashley P Jones, Kaitlyn R Chan, Graham Ogg, Alan D Irvine, Carsten Flohr, Leonie S Taams, on behalf of the TREAT trial team, Clinical and Experimental Dermatology, 2025;, llaf301, https://doi.org/10.1093/ced/llaf301
Abstract
Atopic dermatitis (AD) is a chronic dermatosis characterised by type-2 inflammatory responses, skin barrier anomalies, and microbiome dysregulation. The variation of AD presentation necessitates a better understanding of the underlying disease mechanisms and the modulation of immune markers over a treatment course. Globally the most used systemic therapies for moderate-to-severe AD are methotrexate (MTX) and ciclosporin (CyA).
 |
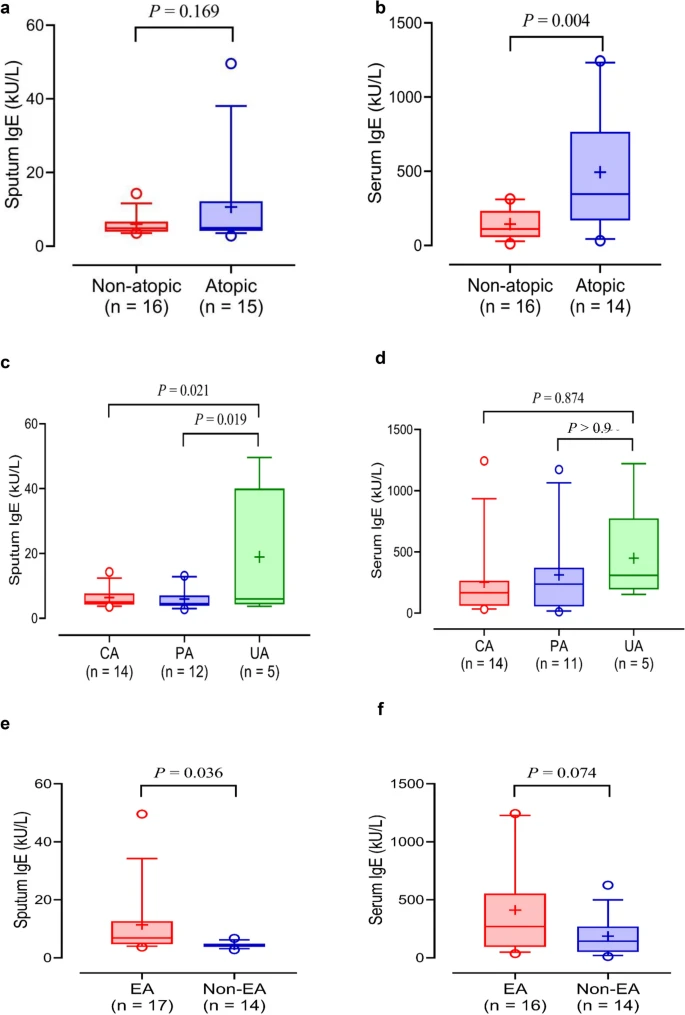
| Gating strategy for identification and analysis of cytokine-expressing CD4+ T 4 cells in peripheral blood from TREAT participants. |