Bachtel ND, Cullen JL, Liu Met al. Science. 2025 Aug 7;389(6760):eadp0246. doi: 10.1126/science.adp0246.
Structured Abstract
INTRODUCTION
Food allergies are a growing medical problem in the industrialized world. In the most extreme cases, allergic reactions manifest as anaphylaxis, a life-threatening state of bronchoconstriction and hemodynamic collapse, which occurs when food antigens enter the bloodstream and activate immunoglobulin E (IgE)–primed mast cells throughout the body. This view has led to diverse models studying anaphylaxis through intravenous administration of food antigens; however, this perspective minimizes the importance of local exposure to food antigens in mucosal tissues in the gut.
RATIONALE
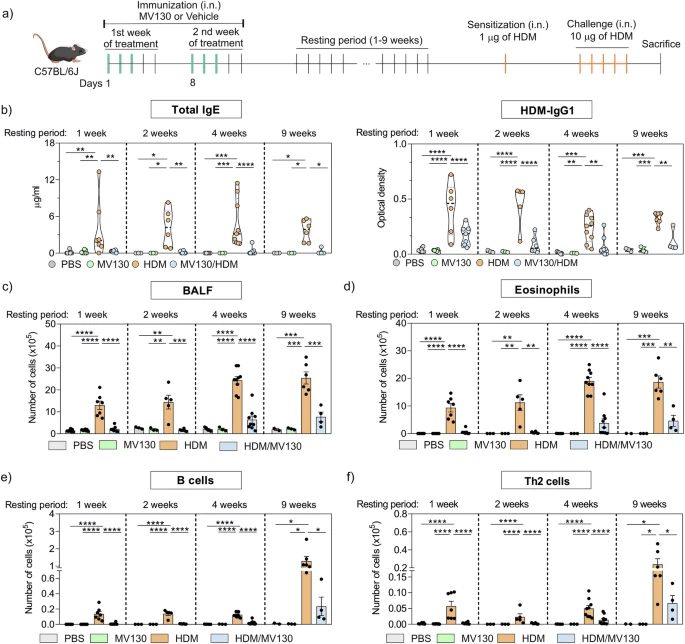
Mouse models of food allergy utilize repeated gastrointestinal administration of allergen, which increases anaphylactic responses to ingestion over time. This hypersensitive state is associated with an increase in the number of mucosal mast cells in the small intestine, and studies utilizing mice deficient in intestinal mast cell expansion suggest that this population is critical for food-induced anaphylaxis to occur. We used bulk and single-cell RNA sequencing, in vitro culture models, and flow cytometry to analyze intestinal mast cell biology and to identify factors governing oral anaphylaxis susceptibility and severity.
RESULTS
 |
| Intestinal mast cell differentiation highlights mediator requirements for oral anaphylaxis |