Lee, E., Lee, B., Krishnan, S. et al. Allergy Asthma Clin Immunol 21, 41 (2025). https://doi.org/10.1186/s13223-025-00981-4Abstract
Background
Unverified drug allergy labels are common and associated with significant patient harm, yet infrastructure and testing practices vary across clinical settings in Canada.
Objective
To characterize variability in drug allergy management among allergists in Canada and identify setting-specific barriers to drug allergy testing and desensitization.
Methods
We developed a peer-reviewed 40-item survey, distributed via the Canadian Society of Allergy and Clinical Immunology, to assess practice patterns, testing modalities, and perceived barriers among allergists. Descriptive statistics and Fisher’s exact test were used to evaluate responses by practice setting.
Results
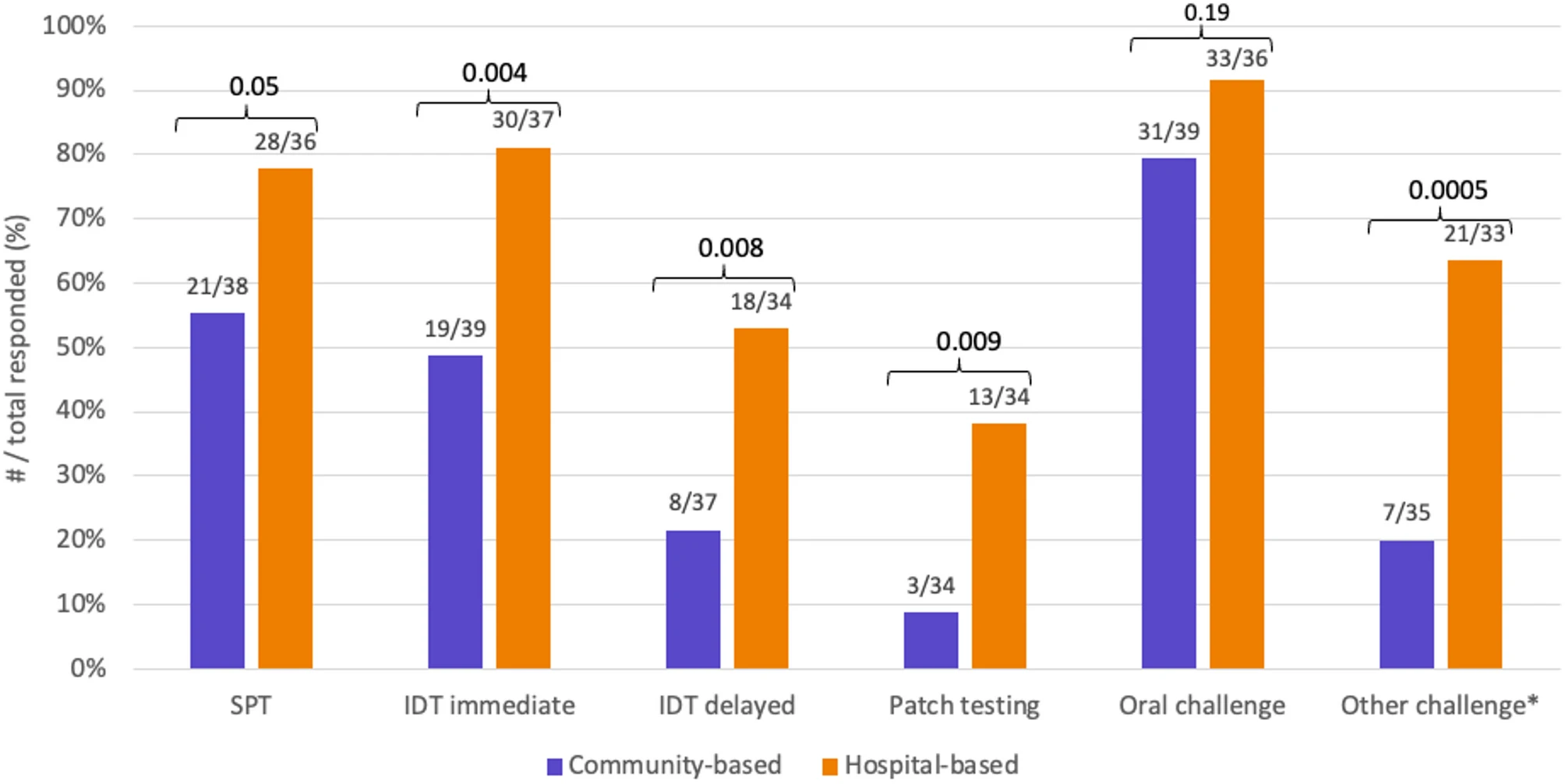
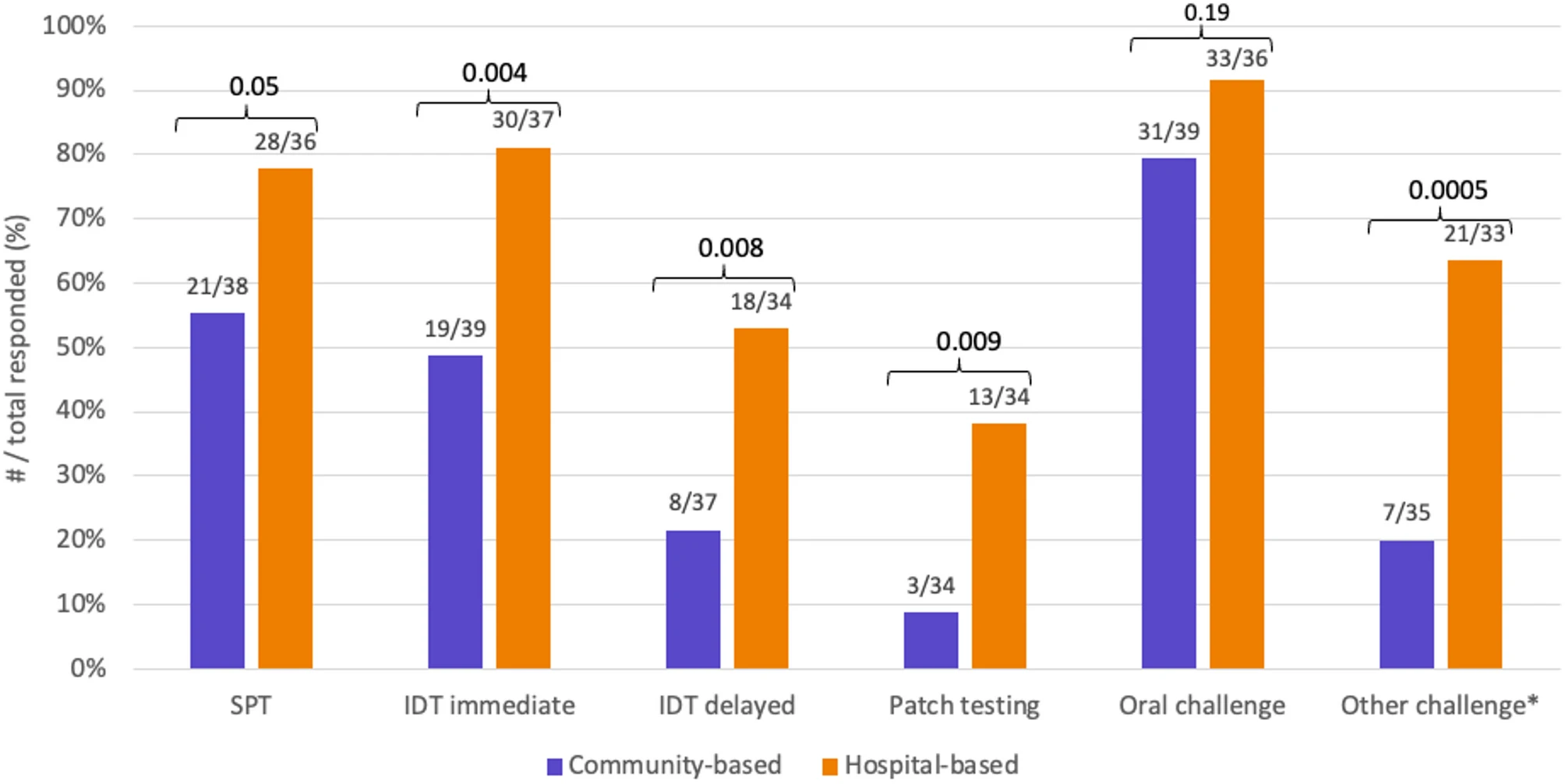 |
| Comparison of drug allergy testing modalities by practice setting |
Sixty-six allergists responded (30% estimated response rate), with 48.4% solely practicing in community clinics and 21.9% solely in hospital-based clinics. While 87.9% performed some form of drug allergy testing, hospital-based allergists were significantly more likely to perform intradermal (81.1% vs. 48.7%, p = 0.004) and patch testing (38.2% vs. 8.8%, p = 0.009), as well as non-oral drug challenges (63.6% vs. 20.0%, p = 0.0005).