- Clinical and Translational Allergy Letter to the Editor
- OPEN ACCESS
Clinical and Translational Allergy 9, Article number: 40 (2019)
Abstract
The Milk Allergy in Primary (MAP) Care guideline was first published in 2013 in this journal. MAP aimed to provide simple and accessible algorithms for UK clinicians in primary care, detailing all the steps between initial presentation, through diagnosis, management and tolerance development. Despite its UK focus, it soon became clear that MAP was being accessed internationally and thus an updated International Milk Allergy in Primary Care (iMAP) guideline was published in 2017. Both guidelines used existing international consensus guidelines to develop accessible algorithms accompanied by patient information leaflets. In 2018, the guidelines were criticised for 3 distinct reasons: promoting the overdiagnosis of cow’s milk allergy (CMA), negatively impacting breastfeeding and the possibility of industry influence on the guidelines. The authors address these criticisms using available evidence and, in the context of this and in consultation with patient groups, members of the General Practice Infant Feeding Network and other infant feeding healthcare leads, have collaboratively produced updated algorithms and an information leaflet to support breastfeeding. We believe iMAP is now closer to its original aim of facilitating early and accurate diagnosis of CMA, whilst minimising, as far as possible, any concerns around overdiagnosis or a risk to breastfeeding rates. We continue to welcome open and constructive engagement about how best to achieve these aims to provide evidence-based, practical guidelines for the primary care practitioner.
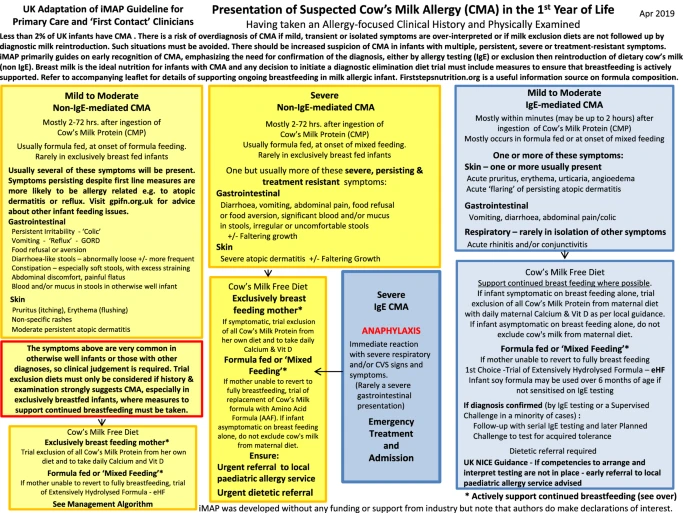 |
| Presentation of suspected cow’s milk allergy (CMA) in the 1st year of Life |
The Milk Allergy in Primary Care guideline was first published in 2013 in this journal by five authors [1], four of whom had been involved in the development group of the UK National Institute for Health and Care Excellence (NICE) 2011 clinical guideline on the ‘Diagnosis and assessment of food allergy in children and young people in primary care and community settings’ [2].
The driver for the development of primary care focussed cow’s milk allergy (CMA) guidance was the limitations of the scope of the NICE guideline, which did not include management of food allergy, nor any specific detail relating to the challenges of identifying and diagnosing milk allergy, which can present with diverse clinical symptoms, due to either an underlying IgE or a non-IgE mediated mechanism. There was good evidence that delay in diagnosis was a common problem for patients, particularly in infants with less severe manifestations of non-IgE mediated milk allergy, and this resulted in a significant [3], unnecessary morbidity and anxiety. This was commonly reported by patients to the authors in their own clinical practice.
The driver for the development of primary care focussed cow’s milk allergy (CMA) guidance was the limitations of the scope of the NICE guideline, which did not include management of food allergy, nor any specific detail relating to the challenges of identifying and diagnosing milk allergy, which can present with diverse clinical symptoms, due to either an underlying IgE or a non-IgE mediated mechanism. There was good evidence that delay in diagnosis was a common problem for patients, particularly in infants with less severe manifestations of non-IgE mediated milk allergy, and this resulted in a significant [3], unnecessary morbidity and anxiety. This was commonly reported by patients to the authors in their own clinical practice.
MAP aimed to provide simple and accessible algorithms for clinicians in primary care, detailing all the steps between initial presentation, through diagnosis and management as well as later follow up to assess for tolerance development, which is almost always seen in early childhood for those children with non IgE mediated milk allergy [1]. In healthcare environments where there is minimal specialist allergy provision, it remains important that mild-moderate non-IgE mediated CMA can be diagnosed accurately and promptly in the primary care setting where these infants are most likely to present. It was considered that a tool which focussed on the UK primary care setting was therefore needed, but soon it became clear that MAP was being accessed internationally, with almost 89,000 accesses to date. This initial guideline was therefore updated in 2017 as International Milk Allergy in Primary Care (iMAP) [4]. Seven further authors, representing five other continents, helped to modify the algorithms such that they could act as a template suitable for local adaptation in different international healthcare settings.
Neither MAP nor iMAP claimed to be the result of new evidence reviews, but instead used the existing international consensus guidelines (such as DRACMA, NIAID, NICE, EAACI, ESPGHAN, BSACI) [5,6,7,8] to develop easy to use algorithms accompanied by a range of patient information leaflets to help support healthcare professionals seeing infants with symptoms which may represent CMA. The diagnostic and management steps in MAP/iMAP were entirely consistent with these guidelines, and the list of symptoms of mild to moderate non-IgE mediated CMA largely repeated the symptoms listed from other guidelines to illustrate the range of potential presentations. In practice, whilst the algorithms were widely distributed, these were often used without the important context provided by the accompanying article. Any algorithm has to balance the accessibility brought by brevity with the reduced clinical context, potentially leading to the less nuanced decision-making that this may bring.
No comments:
Post a Comment