- Letter to the editor
- Open Access
- Allergy, Asthma & Clinical Immunology
Abstract
The concept of the unified allergic airway disease (UAD) recognises the association between allergic inflammation in the upper and lower airways. Patients with asthma and concomitant allergic rhinitis experience more asthma-related primary and secondary care visits. We therefore aimed to determine differences in asthma control (asthma control questionnaire ACQ-6), lung function (spirometry) and T2 biomarkers (FeNO and Eos) in relation to the presence of allergic rhinitis in patients with allergic asthma.
Retrospectively, we evaluated a cohort of 60 consecutive patients with persistent asthma attending our research unit for screening into clinical trials. All included subjects were receiving inhaled corticosteroids (ICS) and had a positive skin prick test (SPT) to at least one common aeroallergen to fulfil the criterion of allergic asthma. Patients with UAD had a diagnosis of allergic asthma in addition to established concomitant allergic rhinitis. T2 biomarkers were significantly higher in patients with allergic rhinitis in contrast to those without. FEV1 % predicted and FEF25-75 % predicted were also significantly lower in patients with concomitant allergic rhinitis. However, there was no difference in ACQ-6 observed between groups. In summary, patients with allergic asthma, the presence of concomitant allergic rhinitis is associated with worse lung function and higher type 2 biomarkers.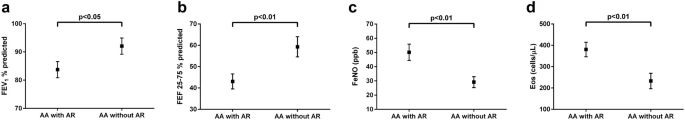
No comments:
Post a Comment