- Research
- Open Access
Abstract
Background
The Allergy Patient Identification for Immunotherapy (AsPIRe) program was a parallel physician and patient survey. The objectives were to examine physician and patient perceptions of seasonal allergy symptoms and their impact on patients, and to examine patient and physician attitudes to allergen immunotherapy (AIT) for seasonal allergies.
AsPIRe was led by a steering committee and received research ethics board clearance from Queen’s University.
Methods
Allergists (17) from across Canada enrolled in the AsPIRe program and completed an on-line survey to collect demographic information and baseline perceptions. Allergists then recruited patients and completed paper-based parallel physician and patient questionnaires. Patients received an AIT informational booklet with their questionnaire. Patients who were AIT-naïve with no contraindication to AIT and 12 years of age and older met the inclusion criteria.
Results
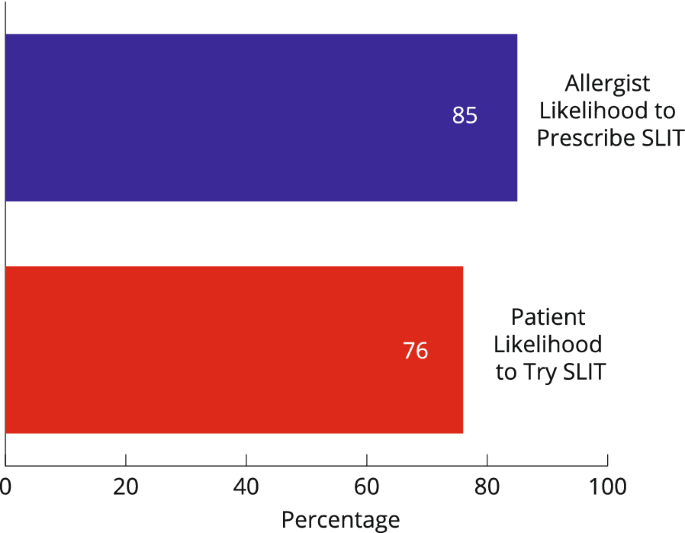 |
| Likelihood to use SLIT: allergist likelihood to prescribe versus patient likelihood to use |
The survey was in field from February 2018 to June 2018. A total of 141 allergist surveys and 136 patient surveys were completed. Mean age of patients was 30 years old (range 12–70). Fifty-seven percent of patients reported prior knowledge of AIT. Seventy-two percent of patients reported seasonal allergies of longer than 5 years duration and in this subset of patients, 46% were at their first allergist visit. Seventy-three percent of all patients indicated they would be likely or very likely to try sublingual immunotherapy (SLIT), if recommended by their allergist compared to 36% for subcutaneous immunotherapy (SCIT). Conversely, 10% of patients reported they would be unlikely or very unlikely to try SLIT compared to 46% of patients who would be unlikely or very unlikely to try SCIT if recommended by their allergist.
Conclusions
In this particular study cohort, there was a gap in perception between allergists and their patients as to the impact of allergy symptoms on daily life. Patients reported being more frequently impacted vs. their physician’s assessment. When asked about preference for AIT options, Canadian patients reported they were more likely to follow their allergists’ recommendation for initiation of SLIT compared to SCIT.
No comments:
Post a Comment