- Research
- Open Access
Allergy, Asthma & Clinical Immunology 17, Article number: 118 (2021)
Abstract
Background
Allergic bronchopulmonary aspergillosis (ABPA) and chronic eosinophilic pneumonia (CEP) both display peripheral eosinophilia as well as pulmonary infiltration, together described as pulmonary eosinophilia, and differentiation is sometimes problematic. This study therefore examined the distinctions between ABPA with and without CEP-like shadows.
Methods
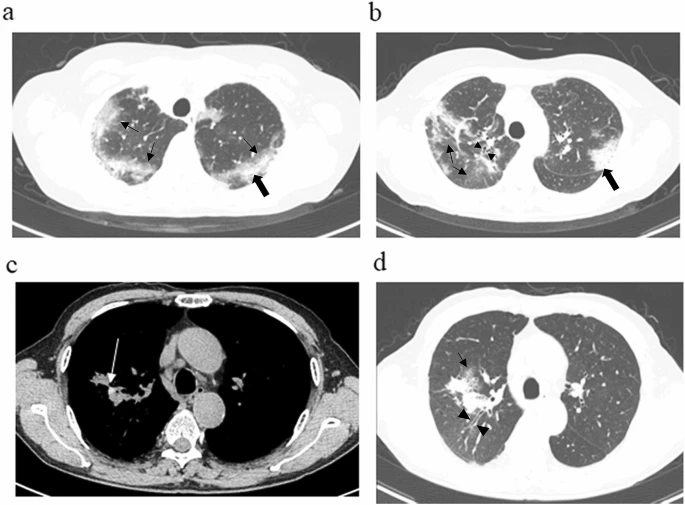
This retrospective cohort study from a single center included 25 outpatients (median age, 65 years) with ABPA diagnosed between April 2015 and March 2019, using criteria proposed by the International Society of Human and Animal Mycology (ISHAM), which focuses on positive specific IgE for Aspergillus fumigatus. Patients were assigned to either the eosinophilic pneumonia (EP) group or Non-EP group, defined according to findings on high-resolution computed tomography (HRCT). The EP group included patients with HRCT findings compatible with CEP; i.e., the presence of peripheral consolidation (p-consolidation) or ground-glass opacities (GGO), with no evidence of high-attenuation mucus. The Non-EP group comprised the remaining patients, who showed classical findings of ABPA such as mucoid impaction. Differences between the groups were analyzed.
Results
Baseline characteristics, frequency of a history of CEP (EP, 50% vs. Non-EP, 26%) and tentative diagnosis of CEP before diagnosis of ABPA (67% vs. 16%) did not differ significantly between groups. Although elevated absolute eosinophil count and Aspergillus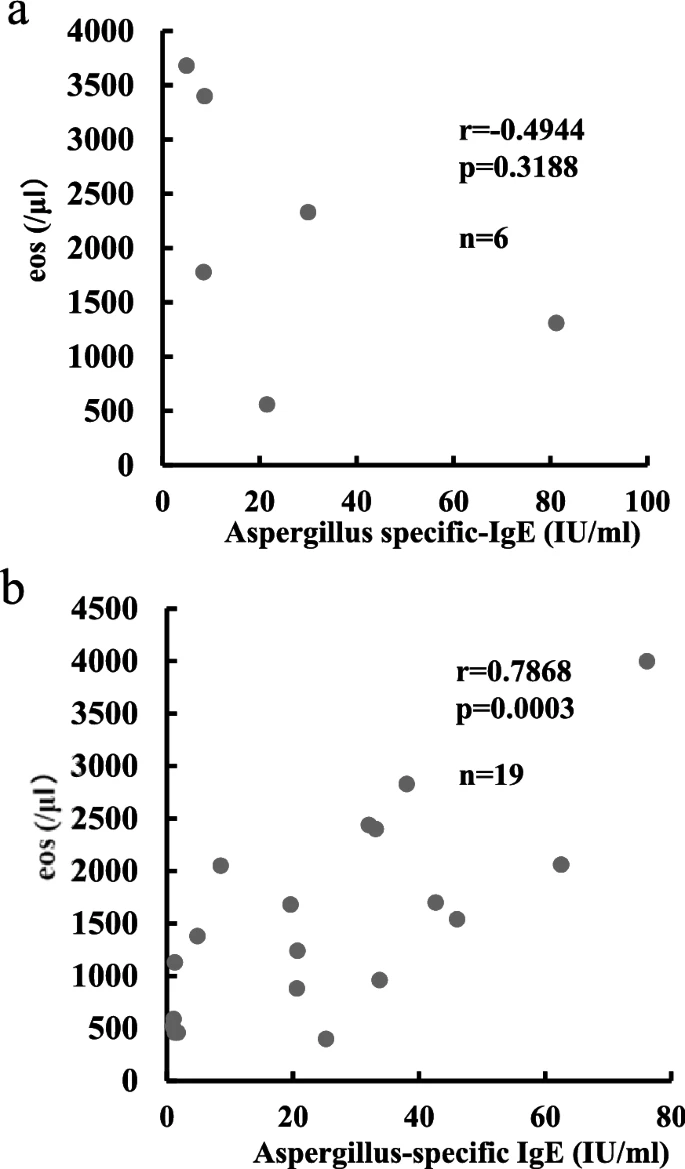 -specific immunoglobulin E titers did not differ significantly between groups, the Non-EP group showed a strong positive correlation between these values (R = 0.7878, p = 0.0003). The Non-EP group displayed significantly higher levels of the fungal marker beta-D glucan (median, 11.7 pg/ml; interquartile range, 6.7–18.4 pg/ml) than the EP group (median, 6.6 pg/ml; interquartile range, 5.2–9.3 pg/ml). Both groups exhibited frequent recurrence of shadows on X-rays but no cases in the EP group had progressed to the Non-EP group at the time of relapse.
-specific immunoglobulin E titers did not differ significantly between groups, the Non-EP group showed a strong positive correlation between these values (R = 0.7878, p = 0.0003). The Non-EP group displayed significantly higher levels of the fungal marker beta-D glucan (median, 11.7 pg/ml; interquartile range, 6.7–18.4 pg/ml) than the EP group (median, 6.6 pg/ml; interquartile range, 5.2–9.3 pg/ml). Both groups exhibited frequent recurrence of shadows on X-rays but no cases in the EP group had progressed to the Non-EP group at the time of relapse.
Conclusions
The ABPA subgroup with imaging findings resembling CEP experienced frequent recurrences, as in typical ABPA. In pulmonary eosinophilia, even if there are no shadows indicating apparent mucous change, the Aspergillus-specific immunoglobulin E level is important in obtaining an accurate diagnosis and in the selection of appropriate therapies for this type of ABPA.
No comments:
Post a Comment