Abstract
Backgorund
Tissue-engineered tracheal grafts (TETG) can be recellularized by the host or pre-seeded with host-derived cells. However, the impact of airway disease on the recellularization process is unknown.
Methods
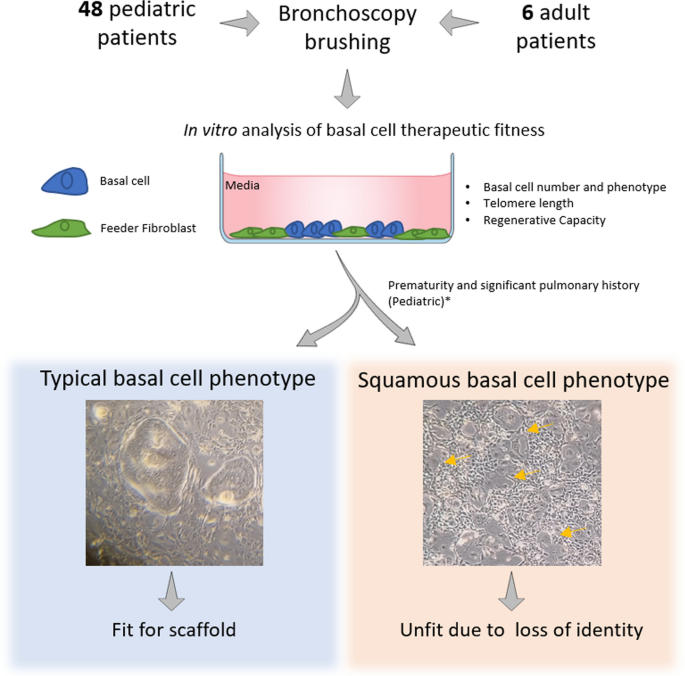
In this study, we determined if airway disease alters the regenerative potential of the human tracheobronchial epithelium (hTBE) obtained by brushing the tracheal mucosa during clinically-indicated bronchoscopy from 48 pediatric and six adult patients.
Results
Our findings revealed that basal cell recovery and frequency did not vary by age or region. At passage 1, all samples produced enough cells to cellularize a 3.5 by 0.5 cm2 graft scaffold at low cell density (~ 7000 cells/cm2), and 43.75% could cellularize a scaffold at high cell density (~ 100,000 cells/cm2).
At passage 2, all samples produced the number of cells required for both recellularization models. Further evaluation revealed that six pediatric samples (11%) and three (50%) adult samples contained basal cells with a squamous basal phenotype. These cells did not form a polarized epithelium or produce differentiated secretory or ciliated cells. In the pediatric population, the squamous basal cell phenotype was associated with degree of prematurity (< 28 weeks, 64% vs. 13%, p = 0.02), significant pulmonary history (83% vs. 34%, p = 0.02), specifically with bronchopulmonary dysplasia (67% vs. 19%, p = 0.01), and patients who underwent previous tracheostomy (67% vs. 23%, p = 0.03).Conclusions
In summary, screening high-risk pediatric or adult population based on clinical risk factors and laboratory findings could define appropriate candidates for airway reconstruction with tracheal scaffolds.
Level of evidence. Level III Cohort study.
Graphical Abstract

No comments:
Post a Comment