Almoqati M, Almasoudi L, Alfaqih Z, et al. (August 17, 2024) Cureus 16(8): e67077. doi:10.7759/cureus.67077
Abstract
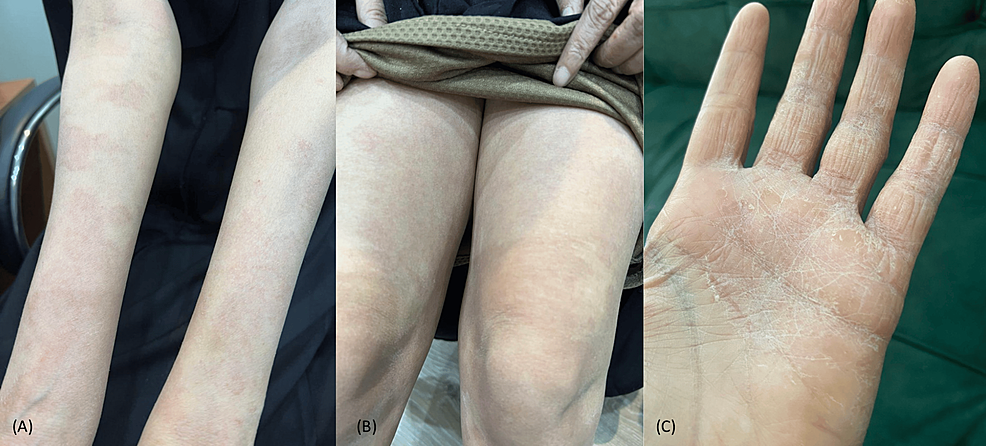 |
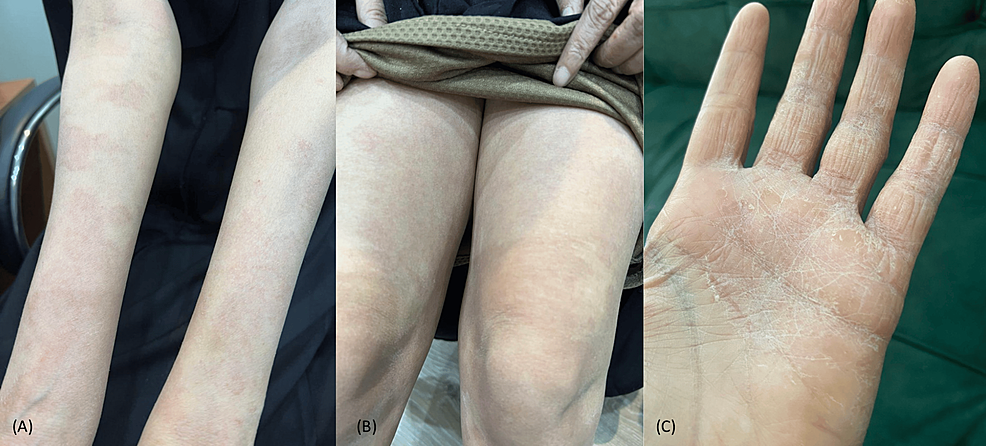
Multiple, diffuse, well-defined, fine, scaly erythematous patches with
an area of spared skin on (A) upper extremities, (B) lower extremities,
and (C) palmoplantar keratoderma |
Pityriasis rubra pilaris (PRP) is a rare, chronic, inflammatory papulosquamous skin disease. Here, we report a case of a 43-year-old female with a known history of atopic dermatitis, bronchiectasis, and goiter who presented with a six-month history of persistent itchy skin lesions on her extremities. A skin examination revealed multiple diffuse, well-defined, fine, scaly erythematous patches with areas of spared skin over all four extremities, along with palmoplantar keratoderma. The trunk was spared. The differential diagnosis included atopic eczema, pityriasis rubra pilaris, dermatomyositis, mycosis fungoides, parapsoriasis, psoriasis, and drug-induced eczematous dermatitis. 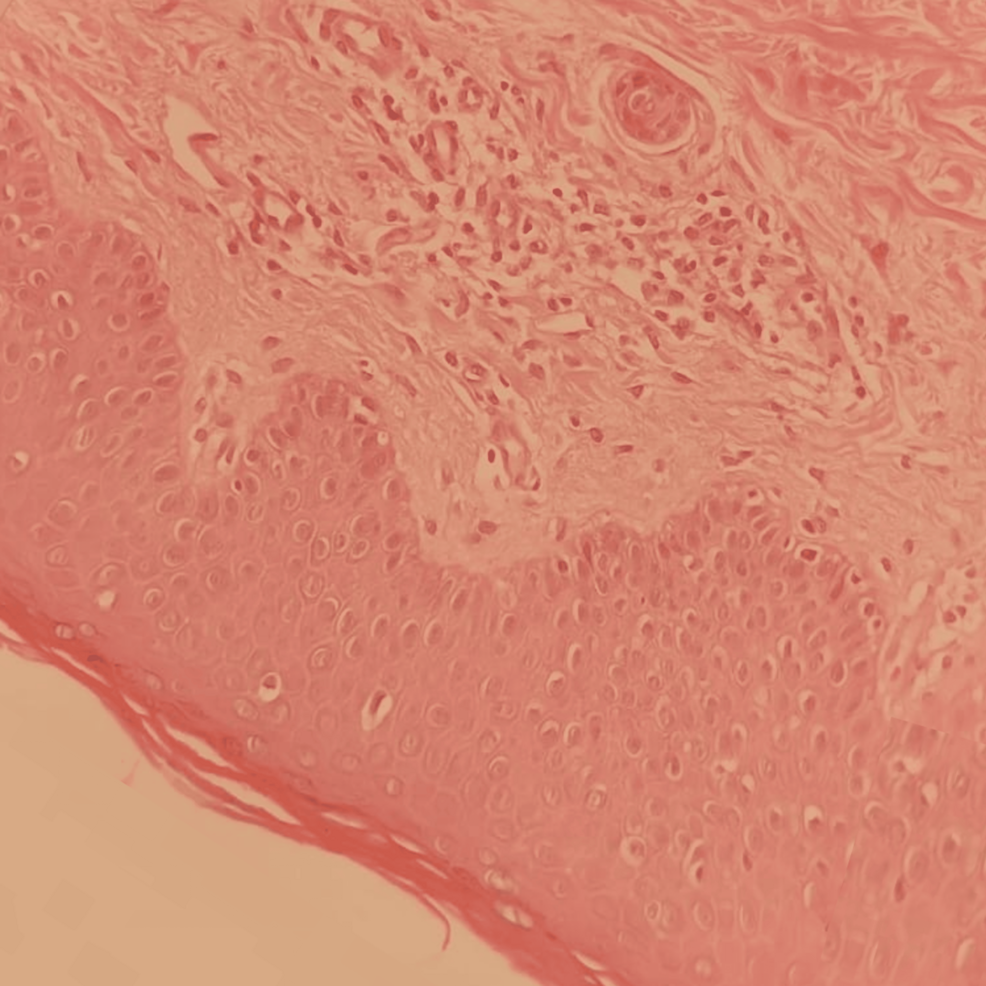 |
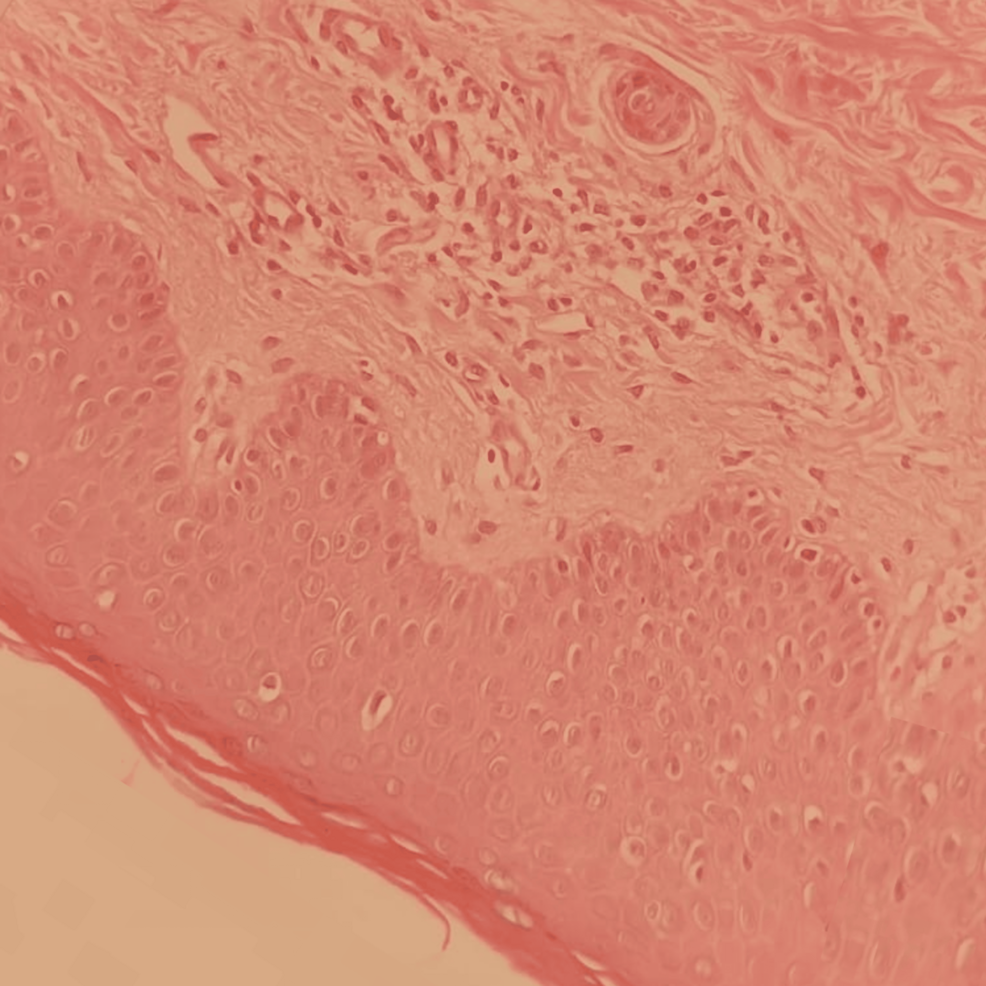
Mild hyperkeratosis, acanthosis, spongiosis, follicular plugging,
and mild perivascular lymphohistiocytic cellular infiltrates in the dermis |
A skin biopsy revealed hyperkeratosis, acanthosis, spongiosis, follicular plugging, and mild perivascular lymphohistiocytic cellular infiltrates in the dermis. Based on the clinicopathological findings, the patient was diagnosed with atypical adult pityriasis rubra pilaris (PRP) (type II). She was started on narrowband UVB phototherapy (NBUVB). Two months after starting NBUVB treatment, all the skin lesions had cleared. She was put under periodic follow-up, and the lesions have remained clear for two years up to the time of this publication.
No comments:
Post a Comment