Adatia, A., Boursiquot, JN., Goodyear, D. et al. Allergy Asthma Clin Immunol 20, 50 (2024). https://doi.org/10.1186/s13223-024-00910-xAbstract
Background
Hereditary angioedema with normal C1-inhibitor function (HAE nC1-INH) and idiopathic angioedema of unknown etiology (AE-UNK) are rare conditions that cause recurrent subcutaneous and submucosal swelling. The characteristics and clinical outcomes of patients with these conditions in Canada have not been studied.
Methods
The aim of this study was to extract real-world evidence from the electronic health records of patients with HAE nC1-INH or AE-UNK who were managed in selected practices of Canadian HAE-treating specialist physicians between 01-Jan-2012 and 01-Jan-2022, to examine case numbers, treatment, clinical outcomes, and healthcare utilization.
Results
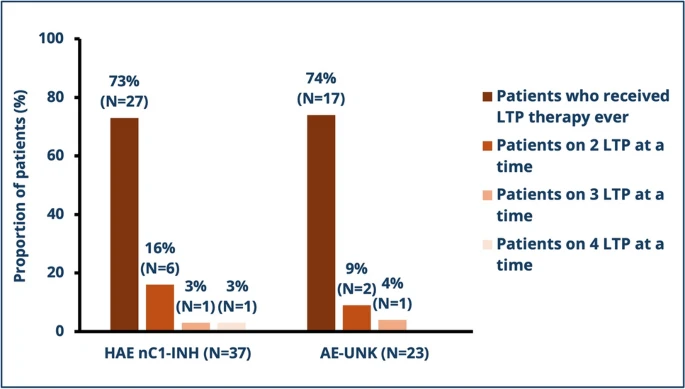 |
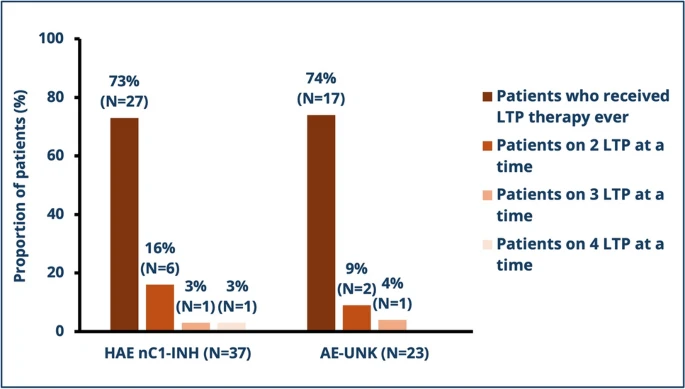
LTP treatment use. HAE nC1-INH, non-histaminergic hereditary
angioedema with family history;
AE-UNK, non-histaminergic hereditary angioedema without
family history |
Of 60 patients (37 with HAE nC1-INH, 23 with AE-UNK), median (range) age at symptom onset was 21.5 (5.0–57.0) and 23.0 (10.0–54.0) years, respectively. Time to diagnosis from onset of symptoms was 7.0 (0.0–43.0) and 2.0 (− 10.0 to 50.0) years. Significant differences were observed in terms of the predominant triggers for angioedema attacks between patients with HAE nC1-INH and AE-UNK: stress (65% vs. 26%, p = 0.007) and estrogen therapy (35% vs. 9%, p = 0.031). Before diagnosis, most patients received antihistamines (50% of HAE nC1-INH and 61% of AE-UNK patients). Post-diagnosis, 73% and 74% of HAE nC1-INH and AE-UNK patients received long-term prophylaxis (LTP), with the most common LTP treatments being subcutaneous pdC1-INH (43% of HAE nC1-INH patients and 39% of AE-UNK patients) and tranexamic acid (41% of HAE nC1-INH patients and 35% of AE-UNK patients). Of patients with HAE nC1-INH, and patients with AE-UNK, 22% and 13%, respectively, were taking more than one LTP treatment concurrently. Before HAE treatment initiation, significantly fewer patients with AE-UNK compared to patients with HAE nC1-INH had angioedema attacks affecting their extremities (13% vs. 38%, p = 0.045) and GI system (22% vs. 57%, p = 0.015). In the three months following treatment initiation, patients with AE-UNK experienced significantly fewer angioedema attacks compared to patients with HAE nC1-INH (median 2.0 attacks [0.0–48.0] vs. 6.0 attacks [0.0–60.0], p = 0.044). Additionally, fewer patients with AE-UNK compared to HAE nC1-INH experienced attacks affecting their GI system (26% vs. 57%, p = 0.032). Attack duration and frequency significantly decreased for patients with HAE nC1-INH from a median of 1.00 day (range: 0.00–7.00) to 0.29 day (range: 0.02–4.00; p = 0.001) and from 10.50 attacks (range: 0.00–90.00) to 6.00 attacks (range: 0.00–60.00; p = 0.004) in the three months following HAE treatment initiation.Conclusions
Using Canadian real-world evidence, these data demonstrate differing clinical trajectories between patients with HAE nC1-INH and AE-UNK, including diagnostic delays, varied attack characteristics, treatment responses and healthcare utilization. Despite treatment response, many patients still experienced frequent angioedema attacks. These results suggest an unmet need for treatment guidelines and therapies specifically for patients with HAE nC1-INH and AE-UNK and better understanding of the pathophysiology accounting for the reported differences between the two.
PDF

No comments:
Post a Comment