Ha, E., Kwak, J., Kim, J. et al. Sci Rep 15, 6038 (2025). https://doi.org/10.1038/s41598-025-89095-w
Abstract
The study aims to investigate the link between paraben exposure, Staphylococcal enterotoxin IgE sensitization, and their combined relationship on allergic rhinitis and nasal patency in children. We assessed 276 children aged 10–12, examining their demographic backgrounds, atopy status, prevalence of allergic diseases, and serum specific IgE levels for Staphylococcal enterotoxins A, B, and toxic shock syndrome toxin (TSST). Parabens metabolites in urine samples were measured to assess exposure levels. The cohort included 276 children (mean 10.9 years), comprising 119 males and 157 females. Of these, 157 children (57.7%) were diagnosed with allergic rhinitis, 44 (15.9%) tested positive for Staphylococcal enterotoxins A, 33 (12.0%) for Staphylococcal enterotoxins B, and 94 (34.1%) for TSST. Propyl paraben was significantly associated with greater TSST-IgE concentrations in the highest quartile (aOR: 2.578, 95% CI 1.275 to 5.212, P = .008) and ethyl paraben showed similar associations in the highest quartile (aOR 2.637; 95% CI 1.223 to 5.669. P = .013). No significant associations were found with other paraben metabolites. Increased propyl paraben levels were linked to greater nasal airway patency, but no direct link to allergic rhinitis was observed. Participants with elevated TSST-IgE concentrations showed a higher odds ratio for allergic rhinitis (aOR: 1.808; 95% CI 1.054 to 3.100, P = .0.032). We observed a significant association between Staphylococcal enterotoxin IgE sensitization and paraben exposure in children. This association might influence allergic rhinitis and nasal response to decongestants, enhancing our understanding of environmental factors in pediatric allergies.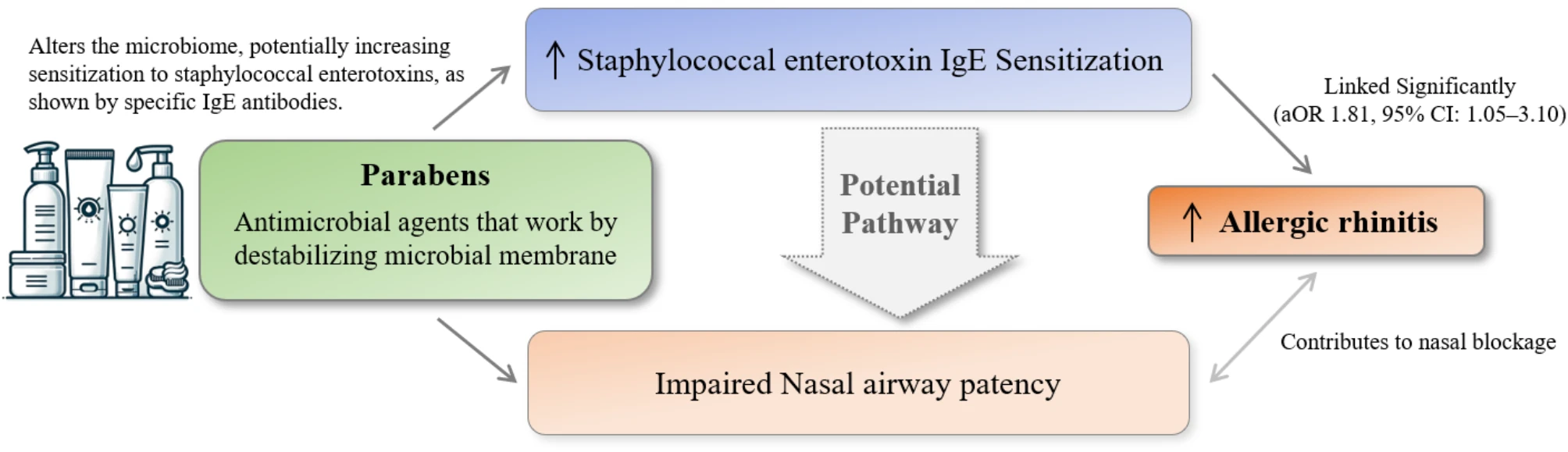
No comments:
Post a Comment