Dahal, A., Chang, W.C., Johansson, E. et al. Sci Rep 15, 17606 (2025). https://doi.org/10.1038/s41598-025-99463-1
Abstract
Staphylococcus aureus (SA) skin colonization in pediatric atopic dermatitis (AD) increases risk for severe AD and development of other allergic diseases. Despite this, there is no consensus regarding the optimal method to detect SA. Studies comparing metagenomic shotgun sequencing (MSS) and culture-based methods in SA detection and relationships to AD outcomes are lacking. In the Mechanisms of Progression of Atopic Dermatitis to Asthma in Children (MPAACH) cohort, we defined SA colonization categories by contact agar plate sampling/culture and skin tape sampling/MSS: double negative, sequencing only positive, contact plate only positive, and double positive (n = 759). 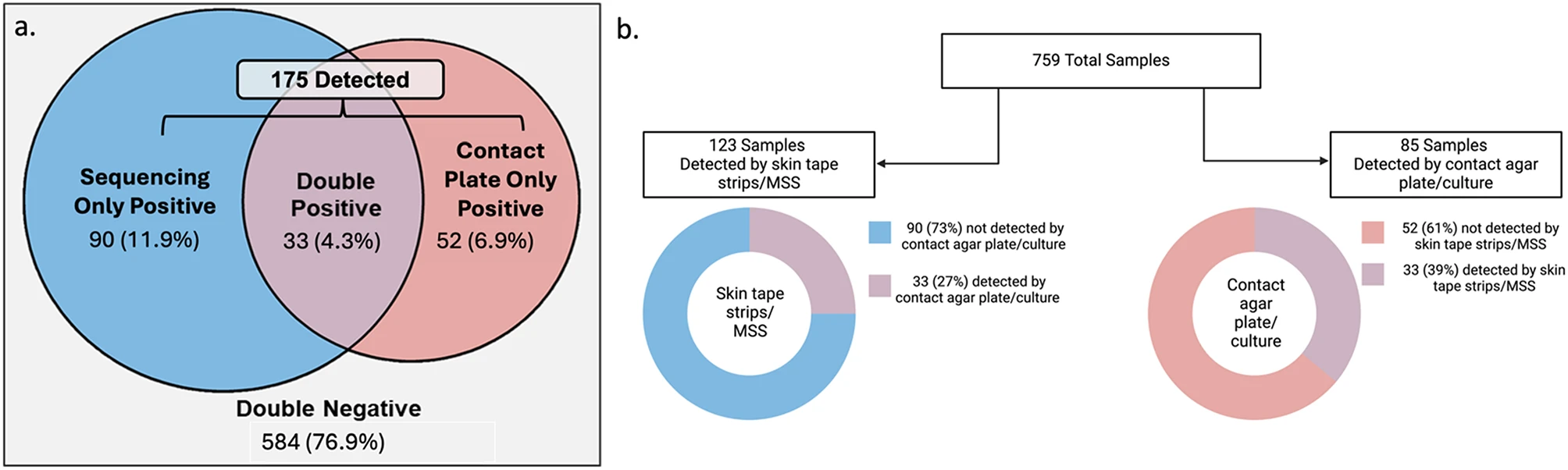
Total samples categories and detection rates by different methodologies
No comments:
Post a Comment