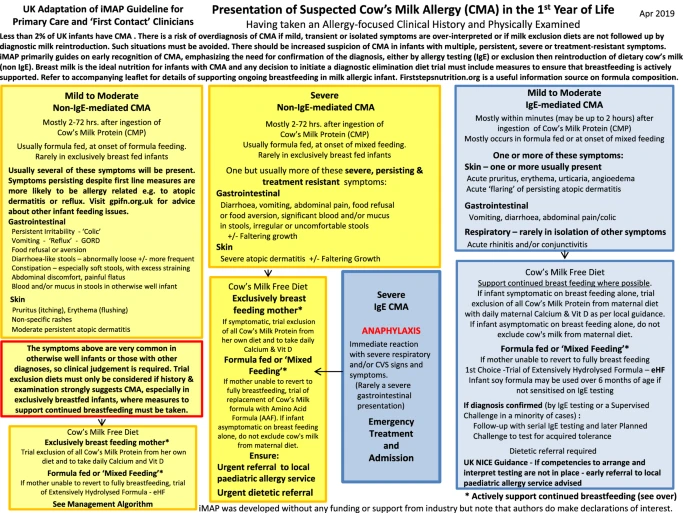
The Milk Allergy in Primary (MAP) Care guideline was first published in 2013 in this journal. MAP aimed to provide simple and accessible algorithms for UK clinicians in primary care, detailing all the steps between initial presentation, through diagnosis, management and tolerance development. Despite its UK focus, it soon became clear that MAP was being accessed internationally and thus an updated International Milk Allergy in Primary Care (iMAP) guideline was published in 2017. Both guidelines used existing international consensus guidelines to develop accessible algorithms accompanied by patient information leaflets. In 2018, the guidelines were criticised for 3 distinct reasons: promoting the overdiagnosis of cow’s milk allergy (CMA), negatively impacting breastfeeding and the possibility of industry influence on the guidelines. The authors address these criticisms using available evidence and, in the context of this and in consultation with patient groups, members of the General Practice Infant Feeding Network and other infant feeding healthcare leads, have collaboratively produced updated algorithms and an information leaflet to support breastfeeding. We believe iMAP is now closer to its original aim of facilitating early and accurate diagnosis of CMA, whilst minimising, as far as possible, any concerns around overdiagnosis or a risk to breastfeeding rates. We continue to welcome open and constructive engagement about how best to achieve these aims to provide evidence-based, practical guidelines for the primary care practitioner.