- Allergy, Asthma & Clinical Immunology Research
- Open Access
Allergy, Asthma & Clinical Immunology 15, Article number: 58 (2019)
Abstract
Background
Allergic rhinitis (AR) is one of the most common diseases globally and usually persists throughout life. In the present study, we aimed to determine whether the expression of inflammatory biomarkers has a relationship with the severity of allergic rhinitis and with comorbid asthma or other allergic diseases in children.
Methods
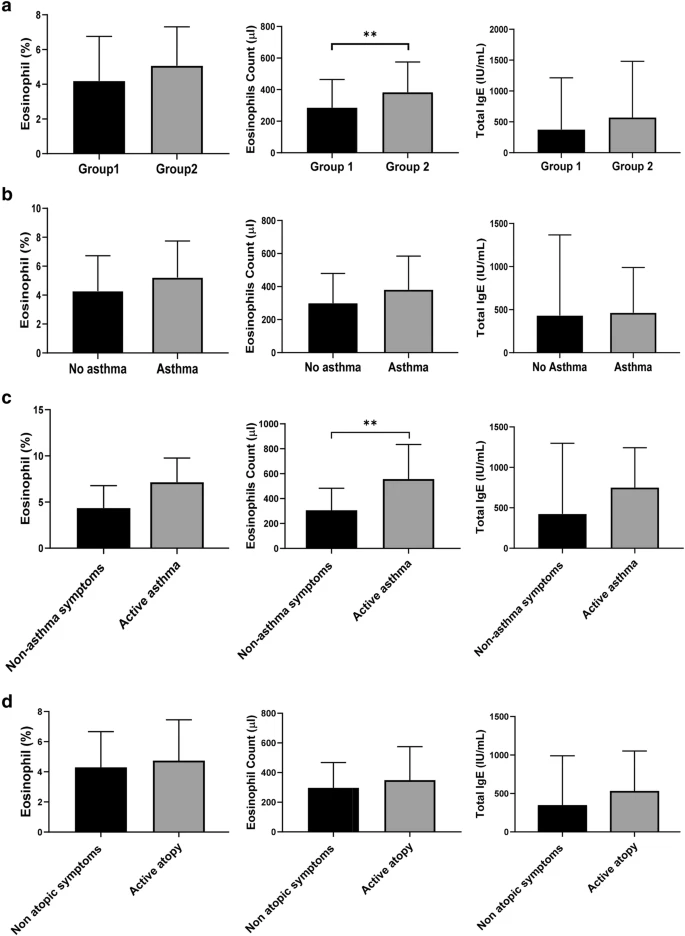
For diagnosis of AR, the skin prick test was performed to measure the responses to 18 allergens. Blood levels of eosinophils and immunoglobulin E (IgE) were examined. We classified the patients into 2 groups based on the severity of the condition as Group 1 [intermittent AR (IAR) or mild persistent AR (PAR)] and Group 2 (moderate to severe PAR). To determine the expression of inflammatory biomarkers, in serum and several biomarkers (caspase-1, IL-1β, CCL-11, CCL-24 and IL-33) were measured in the serum using enzyme-linked immunosorbent assay (ELISA). Additionally, we analyzed the correlation between clinical variables and the expression of biomarkers (eosinophils count, IL-1β and CCL-24) and the severity of AR.
Results
We found that eosinophils count, IL-1β, a marker of activation of inflammasomes, and CCL-24 were significantly increased in the moderate to severe PAR group (p = 0.008, p = 0.003, p = 0.039). Additionally, the expressions of eosinophil count, IL-1β and CCL-24 were significantly higher in patients with active asthmatic symptoms than in those without these conditions. On univariate analysis, allergic rhinitis in sibling, paternal allergic rhinitis, high expression of eosinophils count, IL-1β and CCL-24, history of active asthma and atopy correlated with severity of AR. Multivariate analysis showed only paternal allergic rhinitis and high expression of IL-1β as significant risk factors of moderate to severe PAR with 6.4 fold and 4.7 fold-increase in risk, respectively (p = 0.011 and p = 0.030).
Conclusion
In conclusion, this study provides the first evidence that an excessive release of biologically active IL-1β may promote inflammation in severe PAR. It demonstrates that IL-1β can be a biomarker for active allergic diseases such as AR, asthma, and atopy. Moreover, this finding suggests that IL-1B should be investigated as a therapeutic target in severe PAR and other allergic diseases.
No comments:
Post a Comment