- Research
- Open Access
Allergy, Asthma & Clinical Immunology 18, Article number: 16 (2022)
In the era of COVID-19, utilization of telemedicine has dramatically increased. In addition to reduced travel times, patient expenses, and work or school days missed, telemedicine allows clinicians to provide continued care while minimizing face-to-face interactions, maintaining social distancing, and limiting potential COVID-19 exposures. Clinical Immunology and Allergy (CIA), like many specialties, has adapted to incorporate telemedicine into practice. Previous studies have demonstrated similar patient satisfaction between virtual and in-person visits. However, evidence from fully publicly funded health care systems such as Canada has been limited.
Methods
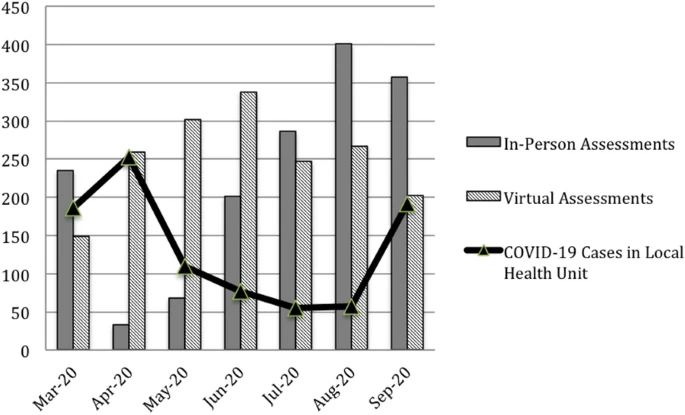
We performed a quality improvement (QI) initiative to assess the feasibility of telemedicine. Between 1 March and 30 September 2020, patient encounters of two academic allergists at a single institution in London, Ontario, Canada were analyzed. Assessments were categorized into in-person or telemedicine appointments. A random sample of patients assessed virtually completed a voluntary patient satisfaction survey. Qualitative analysis was performed on survey comments.
Our quality improvement initiative demonstrated high patient satisfaction and time savings with virtual
No comments:
Post a Comment