Li K, Jin J, Yang Y, Luo X, Wang Y, Xu A, Hao K, Wang Z. Int J Nanomedicine. 2024 Nov 18;19:12015-12037. doi: 10.2147/IJN.S484327.
Abstract:
 |
| Graphical abstract |
A blog that publishes updates and open access scientific papers about allergy, asthma and immunology. Editor: Juan Carlos Ivancevich, MD. Specialist in Allergy & Immunology
Li K, Jin J, Yang Y, Luo X, Wang Y, Xu A, Hao K, Wang Z. Int J Nanomedicine. 2024 Nov 18;19:12015-12037. doi: 10.2147/IJN.S484327.
Abstract:
 |
| Graphical abstract |
Balan, D., Baral, T., Manu, M.K. et al. Allergy Asthma Clin Immunol 20, 60 (2024). https://doi.org/10.1186/s13223-024-00922-7
Abstract
Background
Asthma is a chronic, heterogeneous disease characterized by airway inflammation. Asthma exacerbations significantly increase the disease burden, necessitating new therapeutic approaches. Emerging evidence suggests probiotics, through the gut-lung axis, may benefit asthma management by modulating immune responses and reducing inflammation.
Methods
This systematic review and meta-analysis adhered to PRISMA guidelines and was registered with PROSPERO (CRD42023480098). A comprehensive search of PubMed, Scopus, Web of Science, and Embase was conducted up to March 2024. Inclusion criteria encompassed randomized controlled trials (RCTs) evaluating probiotic interventions in asthma patients. Statistical analysis was done using RevMan 5.3, with odds ratios (OR) and 95% confidence intervals (CI) calculated, and heterogeneity assessed using I2 statistics.
Results
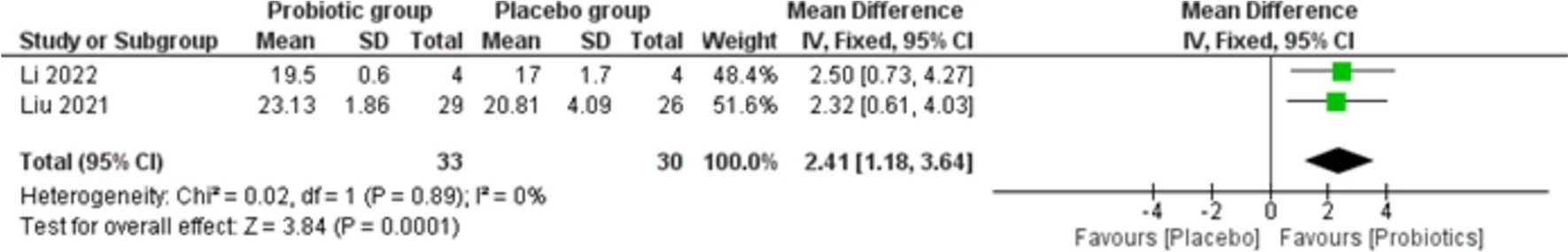 |
| Forest plot for asthma control test |
Conclusion
Probiotic supplementation may be beneficial in improving asthma symptom control with no significant impact on lung function indices or eosinophil levels. Probiotics can be a potential adjunctive therapy in asthma management, particularly for asthma symptom control.
Abstract
 |
| a, b Key cells in AR and their pathology. |
Abstract
 |
| Process of the 40-year-old male patient diagnose as TEN. |
Objectives: This study aimed to report the clinical outcomes of different types of SCARs treated with TNF-α inhibitors.
Santos AF, Riggioni C, Agache I, et al. Allergy. 2024; 00: 1-23. doi:10.1111/all.16345
Abstract
 |
| Management of IgE-mediated food allergy. |
This European Academy of Allergy and Clinical Immunology (EAACI) guideline provides recommendations for the management of IgE-mediated food allergy and was developed using the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach. Following the confirmation of IgE-mediated food allergy diagnosis, allergen avoidance and dietary advice (with support of a specialised dietitian, if possible) together with the provision of a written treatment plan, education on the recognition of allergic symptoms and prescription of medication including adrenaline using an auto-injector are essential.
Abstract
Idiopathic hypereosinophilic syndrome (IHES) is defined by peripheral eosinophilia of more than 1500 eosinophils/µL for a 6-month duration with signs of organ involvement in the absence of parasitic infection, allergic reaction, or other recognized causes of eosinophilia.
 |
| Portal inflammation with eosinophilic infiltration. |
Key Points
Question What is the efficacy and safety of once-daily roflumilast cream, 0.15%, in patients with atopic dermatitis (AD)?
Findings In 2 phase 3 randomized clinical trials of 1337 individuals with AD, significantly more patients treated with once-daily roflumilast cream, 0.15%, achieved Validated Investigator Global Assessment for Atopic Dermatitis success at 4 weeks than patients treated with vehicle cream. Roflumilast was well tolerated with low rates of adverse events in both trials.
Meaning An effective, well-tolerated, once-daily, nonsteroidal treatment like roflumilast cream, 0.15%, may address several unmet needs and substantially improve the treatment landscape for patients with AD.
Abstract
Importance Safe, effective, and well-tolerated topical treatment options available for long-term use in patients with atopic dermatitis (AD) are limited and associated with low adherence rates.

https://doi.org/10.2147/JAA.S477376
Abstract:
Background: Adenoid hypertrophy (AH) and allergic rhinitis (AR) are common pediatric diseases, seriously affecting the quality of life and growth of children. The recurrence rate of AH is higher for patients with than for those without concurrent AR. Allergen specific immunotherapy (AIT) is the only effective therapy for modifying the course of allergic diseases. This study sought to investigate the efficacy of AIT in preventing AH recurrence in patients with AR who underwent adenoidectomy.
Methods: This study included 134 children aged 5– 12 years with concurrent AH and AR. They were separated into the subcutaneous immunotherapy (SCIT) group treated with a double-mite allergen preparation or the non-AIT group treated symptomatically with only medications. The adenoid/nasopharyngeal ratio at one year after adenoidectomy was used to assess AH recurrence.