Röcken, J., Darie, A.M., Grize, L. et al. BMC Pulm Med 25, 150 (2025). https://doi.org/10.1186/s12890-025-03618-9
Abstract
Background
Inpatient polysomnography (PSG) is the gold standard for the diagnosis of obstructive sleep apnoea (OSA), however, both complexity and costs limit the availability of this examination. Home sleep apnoea testing devices are a diagnostic alternative in patients with increased risk of OSA. We evaluated the diagnostic performance of a Doppler radar technology based, contactless sleep apnoea testing device (CSATD) in a cohort of patients with a clinically increased risk of OSA.
Methods
Monocentric prospective study. Sleep monitoring with the CSATD SleepizOne + without pulse oximetry (Sleepiz AG, Switzerland) was performed simultaneously with elective inpatient PSG. PSG was analysed blinded to the CSATD results and according to AASM 2012 criteria by certified sleep physicians. The CSATD data were analysed automatically and independently by a dedicated software.
Results
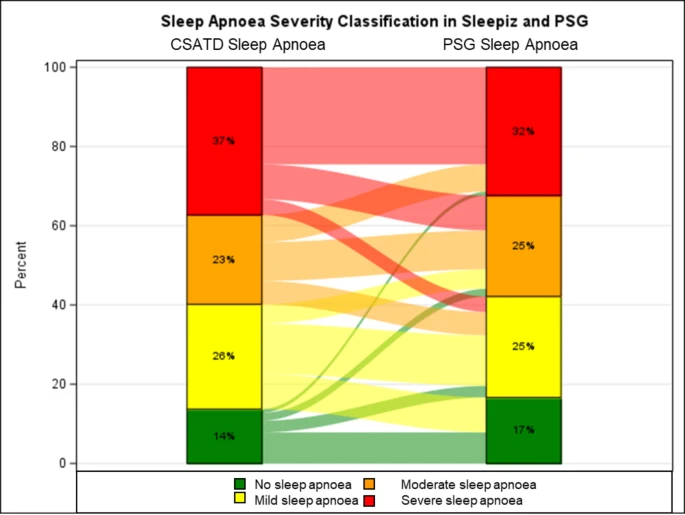 |
| Sankey plot showing sleep apnoea severity classification in both sleep studies (CSATD and polysomnography (PSG)). CSATD: Contactless sleep apnoea testing device |
Conclusion
CSATD accurately identifies patients with OSA, particularly using an AHI threshold of ≥ 15/h. However, it performs subpar in disease severity stratification.

No comments:
Post a Comment